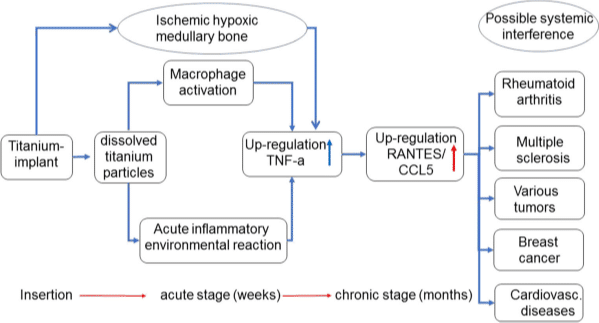
Metallic implants placed in humans exhibit wear and corrosion that result in the liberation of metal-containing by-products. In the case of titanium (Ti) containing implants, the metal containing debris may exist in a number of states, including metallic particles produced by mechanical wear and the products of metal corrosion in biological environments, such as the joints and surrounding fluids and tissues.
Tag Archives: Emerginnova
Titanium implants are routinely used for bone fractures as well as dental work. It has recently been shown that titanium-based implants both corrode and degrade, generating metallic debris. There is some concern over the increased concentrations of circulating metal-degradation products derived from these implants, and their potential harmful biological effects over a period of time, including hepatic injury and renal lesions.
This review is based on current titanium research demonstrating the many factors that can pose a negative impact on human health when exposed to the various forms of titanium, including its relationship and interactions with other metals.
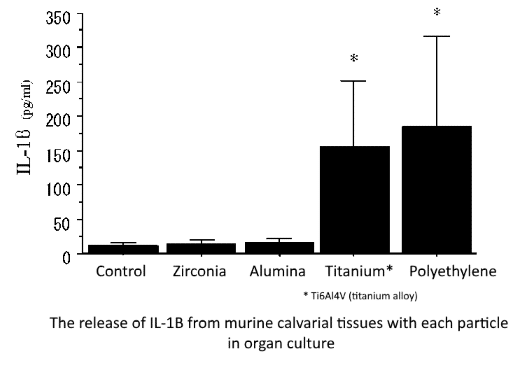
The inflammatory response and bone resorption induced by ceramic particles were much smaller than those induced by polyethylene and Ti6Al4V. These biological features suggest the biocompatibility of ceramics as a joint surface material for artificial joints.
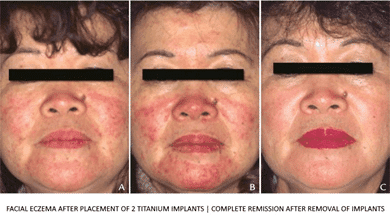
This review of the literature indicates that titanium can induce hypersensitivity in susceptible patients and could play a critical role in implant failure.
Nickel in the alloy NiTi induced an increase in the toxic potential compared to Titanium microparticles.
This study indicates that titanium is unsuitable as a biomaterial in devices which are in direct contact with blood for a prolonged period.
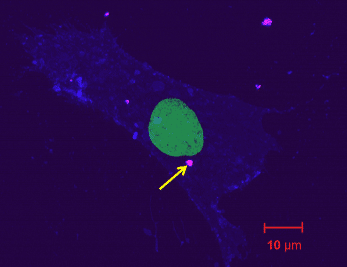
Cell viability is negatively correlated with titanium concentration. Further, titanium debris might lead to an inflammatory biologic response of dental peri-implant tissue.
Recent data support the implication of accelerated titanium dissolution products in peri-implantitis. It is unknown whether these dissolution products have an effect on the peri-implant microbiome, the target of existing peri-implantitis therapies.
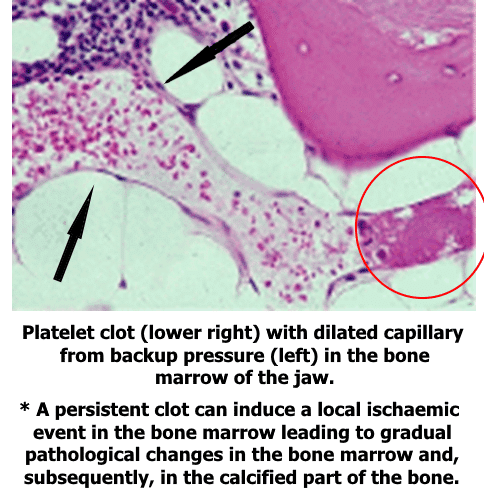
Ischaemic hypoxic medullary bone occurs when there is a disruption in the vascular supply of that bone tissue. Such disruption can occur when a thrombus (clot) is formed and does not subsequently break down (fibrinolysis).