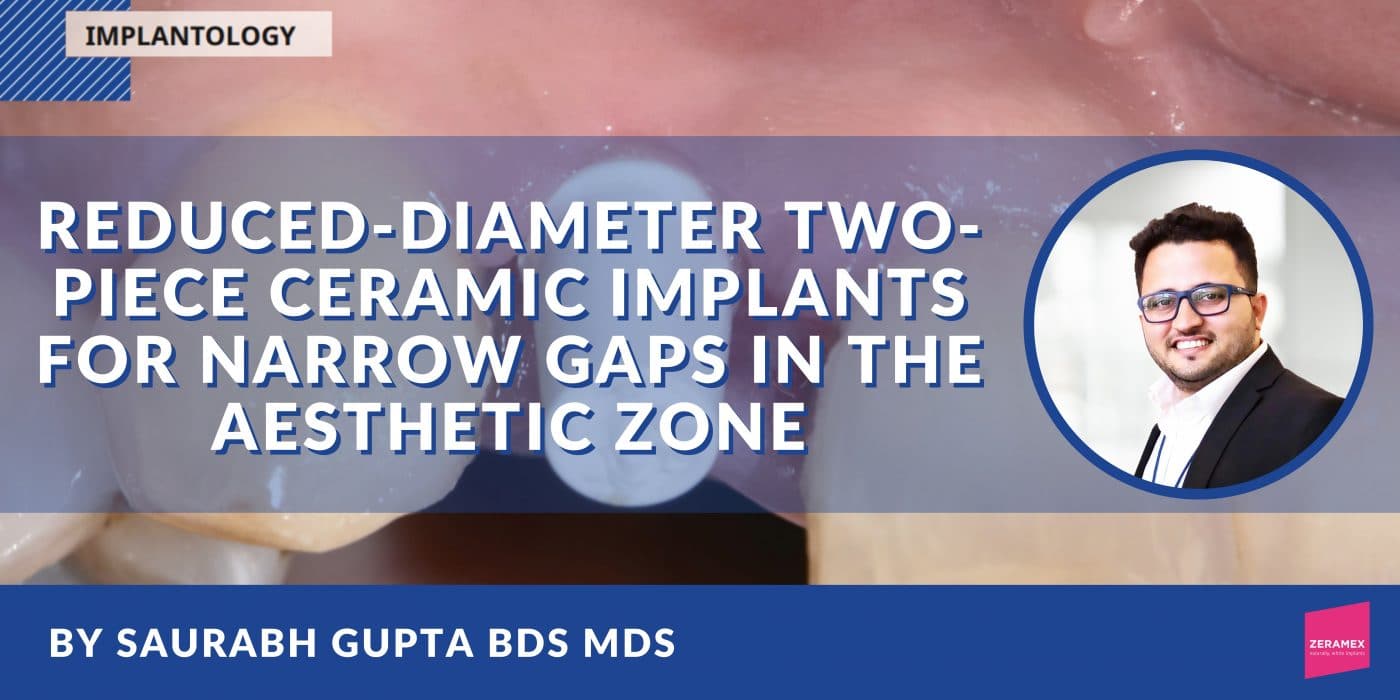
Reduced-diameter two-piece ceramic implants for narrow gaps in the aesthetic zone
By Dr. Saurabh Gupta BDS, MDS
Zirconia implants are one of the most innovative and exciting developments in dental implantology. Studies have shown that zirconia implants cause little to no inflammation of the peri-implant tissue while prolonging the epithelial attachment. In addition, these implants look more natural and therefore offer improved aesthetics.
Introduction
Some of the modern ceramic implant systems, such as the Zeramex XT (Dentalpoint AG, Switzerland), completely dispense with metal components, which makes them ideal for people with titanium or metal intolerance and an adequate alternative for patients who want metal-free rehabilitation with implants prefer [1-3]. Aesthetics can be a challenge even under normal circumstances and around natural teeth. If teeth are to be replaced by implants, especially in the aesthetic zone, the prevailing gingival conditions can have a negative optical impact on the desired long-term result. Thin and / or transparent gum tissue, known as the “thin gingival biotype”, allows the implant to shine through. This leads to a darker gingiva in this area and thus reduces the aesthetics of the patient’s smile. If an anterior tooth is missing over a longer period of time, the facial bone portion is resorbed and the remaining bone thickness available for the implant is reduced in this portion of the alveolar ridge. This leads to a dark shadow even in patients with thicker soft tissue peri-implant does not optically merge with the tissue of the adjacent natural teeth [4-7]. A clinical case is described below that demonstrates the use of a two-part reversibly screw-retained ceramic implant with a reduced diameter in the aesthetic zone.
Case documentation
The 42-year-old patient presented to our clinic with the request for a replacement for a missing right upper lateral incisor. The tooth had been removed alio loco and the extraction wound had healed completely. Facially, there was already a strong bony retraction, which had arisen as a result of the natural bony breakdown and remodeling processes during the healing process (Fig. 1 and 1a). Further examination showed that when the patient smiled, a relevant part of the gingiva became visible. This could have impaired the overall aesthetic impression in combination with the prevailing thin biotype and the reduced vestibular bone thickness around the implant. Treatment options were discussed with the patient to avoid these visual impairments would let. This included the use of a zirconium oxide implant which, due to the tooth-like color of the material, would prevent a dark discoloration of the thin gingiva from the outset. Alternatively, the insertion of a titanium implant would have been possible, but this would have required additional surgical interventions, such as a connective tissue transplant, to achieve a comparable aesthetic result. By thickening the tissue, one would try to mask the darker area around the implant. After considering the options, the patient opted for the ceramic implant – without the need for a connective tissue transplant.


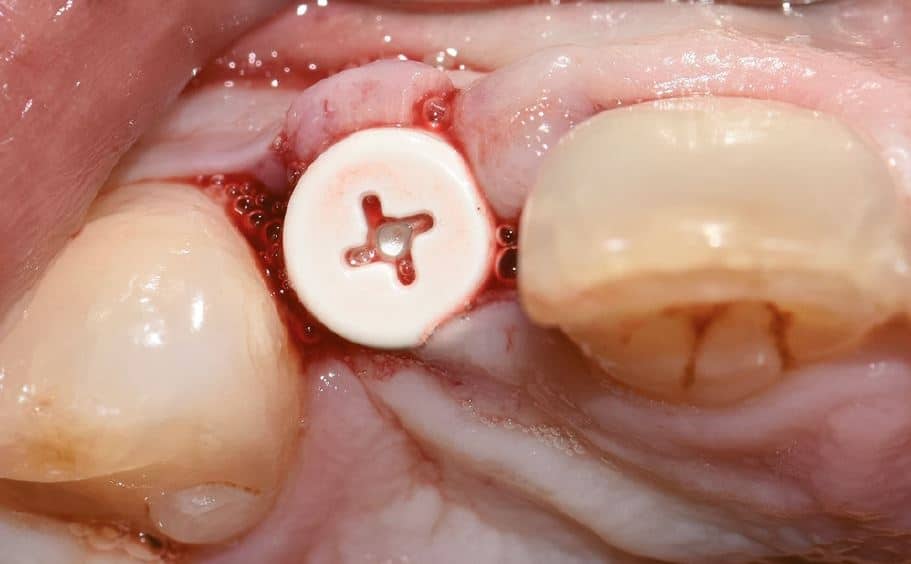
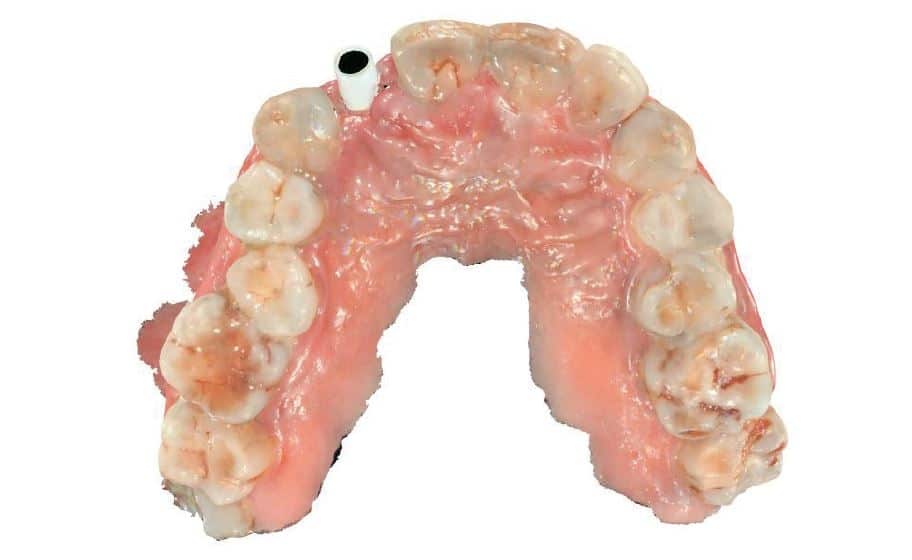
A two-part reversibly screwable zirconium oxide implant (Zeramex XT) made of ATZ (aluminum-toughened zirconia) with a reduced diameter of 3.5 mm and a length of 12 mm was placed under local anesthesia with minimal flap formation, closed with an end cap, the tissue repositioned and sutured (Fig. 2 and 2a).


Surgical phase
The guidelines for the insertion of ceramic implants in the anterior region and the manufacturer’s drilling protocol were followed. Both the vertical and the transverse insertion depth of the implant are decisive for the prosthetic success. The trimodal surface of the Zeramex XT consists of the blasted and etched implant body with a micro and micro roughened surface topography, a smooth area on the implant neck and a purely etched transition zone in between. This type of morphology allows the implant to be placed between 1.6 mm and 0.6 mm supracrestally. This flexibility in the placement of the implant allows adequate vertical implant positioning, which is determined by the height of the gingiva and the existing bone around the neighboring teeth.
Soft tissue management and final prosthetic restoration
After the healing phase was completed, the implant was exposed with a 940 nm diode laser. The healing cap was then removed and a standard Zeramex healing cap was used for the initial soft tissue shaping for a period of two weeks. (Fig.3)
There was no evidence of inflammatory changes in the patient, which proves the excellent biocompatibility and host response (Fig. 4 and 5). A Zeramex standard abutment also made of ATZ was fixed in the implant with a Vicarbo screw (Zeramex XT) (Fig. 7). This screw made of carbon fiber reinforced high-performance plastic ensures a balanced power transmission of the forces that occur during operation. In order to keep the tissue around the implant stable, a digital impression was taken with the scan body belonging to the system in order to avoid unnecessary manipulation for the production of the temporary and final crown (Fig. 5a and 6a). The temporary restoration was fixed over a period of one week, followed by the insertion of the final zirconium oxide crown (Fig. 8). The all-ceramic crown was attached to the abutment with a glass ionomer cement.






Discussion
Clinically – but also in the literature – there are increasing reports of complications in the use of titanium dental implants as well as increasing incidences of peri-implant mucositis and periimplantitis, which can affect both the short and the long-term survival rate of titanium implants. The osseointegration rate of the alternative made of zirconium oxide is comparable to that of titanium, but it also shows a superior soft tissue stability and also in the long term a lower affinity for the adhesion of plaque or biofilm. When using titanium implants, regardless of whether the restoration was made on the basis of titanium or zirconium oxide abutments, color differences compared to the soft tissue around natural teeth can be observed – even if zirconium oxide shows a better color match than titanium. This can be transferred to the color of the implant and the associated influence on the overall aesthetic impression: The white color of the implant eliminates any possibility of darkening the gum tissue. The light-optical properties of the ceramic allow light to be transmitted into the deeper tissue, which is similar to that of the natural tooth, thus delivering an aesthetic end result.
However, when planning and performing implant therapy, the bony supply or the available space to neighboring structures must also be taken into account [8]. In this case, the distance between the teeth delimiting the gaps and the thickness of the vestibular bone lamella would not have been sufficient for larger implant diameters. A reduced implant diameter of 3.5 mm was developed for the Zeramex XT system precisely for these situations. The use of this type of implant is limited to narrow gaps in the lower jaw front and for lateral incisors in the upper jaw. Despite the narrow implant body, it was possible to use the same implant interface with the same Vicarbo screw in the interests of stable anchoring of the abutment in the implant and optimal application of force. as with the larger versions with a diameter of 4.2 mm (RB) and 5.5 mm (WB). In this way, even with the narrow implant diameter (SB), the same stability is achieved as with the standard types. The very positive clinical results with two-part ceramic implants after more than ten years make you want more. But long-term studies are also necessary to further verify the effectiveness and success rates of zirconia implants.

Conclusion
The result of this treatment concept is natural aesthetics with no gingival color changes in this thin gingival biotype and without the need for a transplant to mask the implant in the bone (Fig. 9).
DENTALE IMPLANTOLOGIE (Issue 7) | November 2021 | pg. 428 – 431
Pictures, unless otherwise stated: © Gupta
About the Doctor
Dr. Saurabh Gupta
FOUNDER AND DIRECTOR, WHITEZ DENTAL CLINIC EDUCATION DIRECTOR, IAOCI, USA
Dr. Saurabh Gupta has a Master’s Degree in Oral & Maxillofacial Surgery from RGYHS College, Bangalore. He completed his graduation at the renowned Manipal College of Dental Science, Manipal, India. He is a trained professional in multiple surgical disciplines, which include Digital and Laser Dentistry and Implantology.
He is an international and national lecturer and is the Board Member/Education Director of ‘The International Academy of Ceramic Implantology.’ This academy is the USA’s first body to work on metal-free implantology.
He is a dynamic personality and a member of The Zirconia Implant research Group (ZIRG), which aims to orient and lead research work in the field of metal-free implantology and provide support to established and young clinicians in scientific and clinical research. He is an indispensable part of the ‘Bio-ceramic Division’ at ‘The American Ceramic Society,’ Ohio, US. He is also the Academic Collaborator at IISc (The Indian Institute of Science), Bangalore, working on several significant Research and Development projects.
He is also the ambassador and fellow at ‘The Cleaning Implant Foundation, Germany,’ and the body aims at assessing the quality of products and cleanliness of implant surfaces that are available in the commercial markets. He is a member of the advisory board for ‘The Journal of Oral Ceramic Implantology’ (ISSN2293-7897). He is the clinical specialist at COHO Biotechnology, Taiwan. Currently, he is actively working on several research studies focusing mainly on digital dentistry and implant materials.
WhiteZ Dental, Bangalore, India | + 91 99 1620 3455 | [email protected] | [email protected]
Contact
Want to know more about Zeramex?
Email us at [email protected] with your contact details and we will get in touch with you!
ZERAMEX BROCHURE
Click here to download the Zeramex sales brochure